The BID Initiative Story
Implementing Solutions
Developing and implementing data quality and use solutions
Together with Tanzania, Zambia, and BLN members, BID developed and implemented a comprehensive set of interventions to improve data collection, quality, and use. We first identified a suite of proven interventions spanning data management policies and practices, information system products, and training. Together with end users from all levels of the health system, we collaboratively developed this package of interventions for use in Tanzania and Zambia, then piloted the interventions in select facilities and regions before further rolling out.
Based on a literature review and landscape analysis of previous, relevant projects and in close partnership with Tanzania and Zambia, BID identified a holistic package of interventions that could be replicated and adapted in other countries to improve immunization service delivery. These included:
- An electronic immunization registry with supply chain information.
- Automated, simplified report generation.
- Data use campaigns.
- Micro-training videos.
- Peer support networks.
- Barcodes or QR codes on child health cards and vaccine supplies.
- Targeted supportive supervision for health workers.
- Data visualizations/dashboards to monitor facility and neighboring facility performance.
Developing electronic immunization registries
In a scene characteristic of most health facilities across developing countries, bulky paper records overflow from bookshelves and tower above desks, sometimes hiding the health workers seated behind them. Inside each record are rows and rows of patient data. Searching for a child’s immunization history in one of these books is like looking for a needle in a haystack. Electronic immunization registries (EIRs) replace this cumbersome system of manual recordkeeping and have been a critical component of BID’s intervention package. EIRs help ensure that every child is registered for immunization from birth and receives all recommended vaccines. By providing timely, accurate, and complete data, EIRs also empower health workers, so they can do their jobs more effectively and efficiently.

PATH/Trevor Snapp. A health worker sifts through folders at Kaoleni Health Center in Arusha, Tanzania.
The BID Initiative supported development of an electronic registry for each country, which required intensive, sustained collaboration by our team, the governments of Tanzania and Zambia, health workers, and our technical partners. The success of the software development process hinged on documenting and applying knowledge of many factors, such as:
- In-depth knowledge of routine immunization services, clinical care, and vaccine schedules in each country.
- An understanding of micro-level, individual-level data that feed into the EIR as well as macro-level data on system outputs.
- Knowledge about the ways in which data may be used to improve immunization service delivery at each level of the health system.
- Understanding and awareness of the landscape of information system strategies and tools in the country and established standards to ensure EIR data can be shared with other systems (such as District Health Information System 2, or DHIS2).
New technology entails a learning curve, particularly among health workers who’ve used paper registries throughout their careers. The EIRs introduced under BID were no exception. Active engagement of local stakeholders at all steps of the process was critical to ensure that the EIRs were truly functional and enhanced in-country skills related to data quality and use. We established user advisory groups (UAGs) in both Tanzania and Zambia, composed of staff from every level of the health system, to define data needs, refine innovations, and plan rollout strategies.
In one UAG meeting in Zambia, for instance, members were split into small groups and provided with tablets to test early prototypes of the EIR. UAG members buzzed with excitement as they crowded around the screens. They practiced registering children using mock data, entering names, place of residence, date of birth, and weight, and modeled the process for high-volume clinics, where 50 or more children may be seen in a single day. The first attempts were not without trial and error, but UAG members quickly mastered the system, and their feedback informed future iterations of the EIR.
Recommendations and lessons learned: Electronic immunization registries
“It was important for all these new interventions to be tested. After testing, we had a better understanding of which interventions would be helpful and would provide solutions to our immunization challenges.”
– Dr. Cliff Hara, Chairperson of Zambia’s User Advisory Group, District Director of Health
Integrating change management
One of the main criticisms of many efforts to implement new digital tools is that they do not adequately address socio-technical factors—that is, they do a poor job of addressing human aspects of intervention adoption. Applying change management practices ensures that digital health technologies are adopted and integrated within existing processes and cultures of health facilities. For the BID Initiative, change management has complemented implementation of the EIRs. For example, using WhatsApp, health workers connected with their peers from other facilities to troubleshoot filling out monthly reports and ensure sufficient vaccine supply.
Recommendations and lessons learned: Change management
Engaging users to iterate and adapt a registry for Tanzania
In Tanzania, the BID Initiative and the Ministry of Health, Community Development, Gender, Elderly, and Children (MOHCDGEC) teamed up with technical partners to develop the first iteration of their EIR, the Tanzania Immunization Information System (TIIS). The TIIS was an adaptation of an open source platform, GIIS, that was designed and developed to be able to share data with other systems through standards-based data definitions and application programming interfaces (APIs). Because of the complexity of the solution being developed, the timeline for developing TIIS had to be extended from three months to six months—a lesson that was considered in subsequent EIR development.
Pilot use of TIIS, however, showed a need for improvements. The system was slow and frequently crashed, making it difficult for health workers to keep up on busy clinic days. The system also had challenges with synchronization, which led to problems with data integrity and use among facilities using multiple tablets. These challenges and user input led to the decision to seek a tool that would better meet the needs identified for data collection.
In late 2016, TIIS was followed by an improved EIR, the Tanzania Immunization Registry (TImR). TImR provides each health worker with a unique login, offers better synchronization, and enables health workers to order vaccine stock directly through the information system. Its summary reports and colorful data visualizations also help health workers understand and improve upon their performance. TImR effectively manages immunization services by automatically tracking and notifying health workers about the children in their catchment area due for immunization, which vaccines they need, and how much stock and supplies the clinic requires to accommodate these patients. On immunization days, health workers can search for a child record by simply scanning the barcode sticker on each child’s health card and update the child immunization record in the registry.
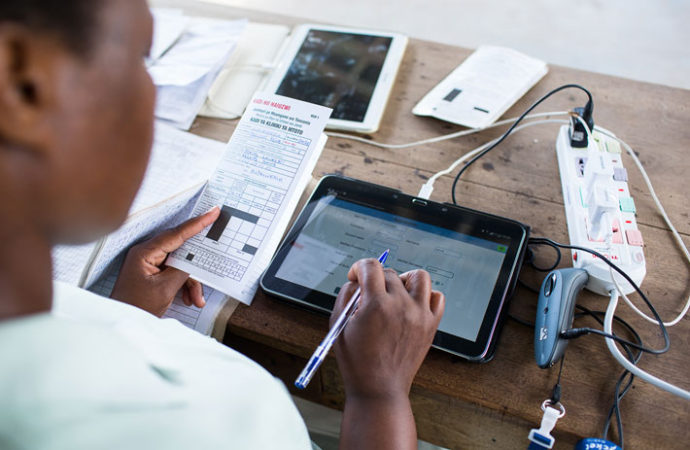
PATH/Trevor Snapp. A health worker navigates a tablet at Usa River Health Center in Tanzania.
The data are accessible at all levels of the health system from the facility level up to the national level, allowing visibility into programs and vaccine stock levels, through interoperability with the Vaccine Information Management System (VIMS) and then to DHIS2. The registry also stores contact information for parents, so health workers can follow up if a child misses a scheduled vaccine. Thanks to the registry’s automated reporting, health workers spend more time delivering care and less time preparing and reporting.
“My clients are very happy, especially when I share with them the reports showing the green color on immunization coverage [which indicates excellent performance], and when they see their children’s electronic cards in the system. They feel the [improvements in] service, as we get more time to discuss their child’s developments. They know that I will follow up, unlike before, since we have all the information at a click of a scanner.”
– Musa Mapunda, a Reproductive and Child Health (RCH) nurse at Makuyuni Dispensary in Korogwe District, Tanga Region, Tanzania.
Although TImR required a new user interface and some additional training, we minimized disruption in Arusha Region, where the previous version of the registry (TIIS) had already been rolled out, by waiting to switch systems until after TImR was successfully implemented in other facilities in Tanga. Thanks to careful planning and precise coordination with Tanzania health officials, data migration was successfully completed in the Arusha Region in early 2018.
Recommendations and lessons learned: Software development cycle